Archive
Physicians and their Employment Agreements
I have posted in the past on the various issues and minefields facing physicians when getting their employment agreement — especially those physicians newly emerging from residency and fellowship programs and entering the so-called “real” world.
In a post yesterday on the KevinMD.com blog, “Only an attorney can operate on your employment agreement”, the author reminds physicians of the need to have a healthcare lawyer assist them in reviewing any proposed employment agreement.
The AMA has also published materials to assist physicians in reviewing their employment agreements.
As physician practice models continue to evolve, there will be increased pressure on physicians to accept what is offered. However, most of the time, problematic provisions are negotiable. And even when they are not, a lawyer can help the physician understand the risks in “taking or leaving it.”
Just as regular people should not try to evaluate their own health situation without help from a physician, physicians should seek professional advice themselves when presented with legal documents. Contracts have meaning and failing to understand what one is signing is like taking someone else’s medication. Benjamin Franklin’s saying that “an ounce of prevention is worth a pound of cure” applies to legal situations as much as to medical ones.
The merging of MDs and DOs: A unification of training standards
From the KevinMd.com blog:
More than a century of American medical history was turned on its ear recently by the announcement that the groups that accredit medical residencies will unify their standards. Don’t be too hard on yourself if you failed to understand the significance (or notice at all). But this should be viewed as good news across the land. As someone who trains doctors from both traditions, I certainly welcome a more level playing field.
It’s about time that there are common standards for MDs and DOs. After all, don’t all states treat allopathic and osteopathic physicians the same and expect them to provide comparable healthcare to their patients? Don’t PI lawyers sue them on the same grounds when there is a bad patient outcome?
Physician Joint Ventured Pharmacies Require Guidance
The pressure is intense on physicians to find additional sources of revenues to balance their losses as a result of reduced reimbursement and other moves to reduce healthcare costs.
In return, physicians are pressuring compounding pharmacies and other healthcare providers for ways to participate in the income stream that physicians and their scripts and referrals produce. There are those who want to put their hands in the pockets of others, and the result is a perfect storm that must be carefully monitored by the legal advisers to physicians and to compounding pharmacies to make sure that EVERYONE complies with the regulatory requirements.
And this is a very fluid environment — what may be acceptable today may not be tomorrow — the OIG’s concerns with PODs and the company-model for anesthesia in ASCs are instructive to physician owned pharmacies..
Florida Healthcare Law Firm Blog
 Florida physicians are being approached to become owners of pharmacies to which they may refer, often compounding pharmacies, but may be unaware of the regulatory issues involved. Physicians need to be aware of the core laws that apply, which include the Florida Patient Self Referral Act (FPSRA), the Florida
Anti Kickback Statute
, the Patient Brokering Act and the Federal Investment Interest Safe Harbor.
Florida physicians are being approached to become owners of pharmacies to which they may refer, often compounding pharmacies, but may be unaware of the regulatory issues involved. Physicians need to be aware of the core laws that apply, which include the Florida Patient Self Referral Act (FPSRA), the Florida
Anti Kickback Statute
, the Patient Brokering Act and the Federal Investment Interest Safe Harbor.
View original post 1,390 more words
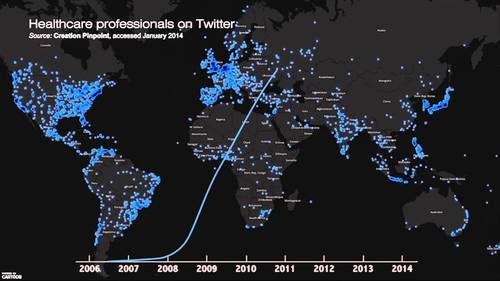
Doctors on Twitter: 2006 – 2014 Worldwide growth mapped #hcsm
[Video maps growth in doctors, nurses and healthcare professionals using Twitter since its launch in 2006 to 2014.]
While Facebook lends itself better as a professional social media portal, it would be interesting to know the growth in patients’ following their physicians on Twitter (and other social media). If we can get past the hurdles of HIPAA restrictions and other legal silliness, social media could become the mechanism through which patients and their physicians effectively interact and improve their healthcare.
See on www.youtube.com
Steps 3, 4, 5, 6, and 7 in Doing a Healthcare Deal (Correctly)
Step 3 – Identify the governmental agencies that have authority over the deal
- Are there any notices or approvals required?
- What are the licensing requirements?
- Will a change in control occur?
- Is a new provider application/number needed?
- Is a CON needed? An inspection?
- What effects will the deal have on any accreditation needed by the parties?
- What is the timing of agency requirements vs. closing the deal?
Step 4 – Identify the third party payors that will be involved
- Are the services to be performed as a result of the deal reimbursed by Medicare?
- Medicaid?
- Other federal or state programs?
- Commercial payors?
- What credentialing/provider applications are needed?
- Do any payors have special requirements that must be satisfied before closing the deal?
Step 5 – Identify the due diligence requirements
Remember that a healthcare deal starts like any other deal, and the parties must do their basic due diligence about each other
- Entity organization and ownership
- Legal authority
- Financial statements, assets and liabilities, liens
- Contracts and commitments, leases
- Employees and benefit plans
- Taxes
- Insurance
- Litigation
Step 6 – Identify the healthcare due diligence requirements
- Licenses and requirements applying to transaction
- Equipment and inventories
- Cost reports, inspections, regulatory correspondence
- Quality of care, malpractice claims/insurance
- Patients records, EHR compatibility, billing software
- Managed care/provider agreements, liability, assignability
- Subcontractors/suppliers
- Stae law requirements
- Fair market value
- Commercial reasonablenessFair market value and Commercial Reasonableness — These are the critical underpinnings of every healthcare deal. What is being given, what is being received, and is it commercially reasonable?Get an opinion from a qualified healthcare valuation expert to support the FMV.
Step 7 – Document the Deal
- Documentation is a critical step in protecting the parties, achieving the goals of the deal, and meeting compliance requirements. Stark Exceptions and Anti-Kickback Safe Harbors impose specific requirements on deal documentation.
- Should the parties enter into a nonbinding letter of intent/memorandum of understanding?
- Pros – helps the parties determine whether there has been a meeting of the minds prior to devoting substantial time and expense and helps manage expectations and reduce surprises.
- Cons – can consume an inordinate amount of time prior to due diligence being completed and lock the parties into unrealistic positions.
Justice Department Hits Physician Owned Distributorships (PODS)
Florida Healthcare Law Firm Blog
 For the first time, the Department of Justice (DOJ) has fired a shot at a
physician owned distributorship
(POD). In the case, the DOJ suit claims that the ownership interest of a neurosurgeon in a spinal surgery device distributorship has caused him to perform unnecessary surgeries.
For the first time, the Department of Justice (DOJ) has fired a shot at a
physician owned distributorship
(POD). In the case, the DOJ suit claims that the ownership interest of a neurosurgeon in a spinal surgery device distributorship has caused him to perform unnecessary surgeries.
PODs have been the source of considerable controversy for years. A couple years ago, they caught the attention of Congress. The Office of Inspector General of the Department of Health and Human Services (“OIG”) has even issued a Fraud Alert making clear their dislike of PODs and sending a clear shot across the bow of those who are in that industry. In 2006, the Office of the Inspector General of HHS and CMS expressed major concerns about PODs, and cited concerns about “improper inducements.” At that time, the OIG stopped short of prohibiting them, but called for heightened scrutiny. CMS itself has stated…
View original post 1,086 more words
Phoning It In – Florida’s Brand New Telemedicine Law
Florida Healthcare Law Firm Blog
 By:
Jackie Bain
By:
Jackie Bain
Until recently, the State of Florida has successfully avoided regulating telemedicine to account for advancements in technology. In 2003, the State issued standards for telemedicine prescribing practice for medical doctors and doctors of osteopathy, but has not formally revisited its position in light of increasingly common telemedicine practice in several states – until now.
Florida’s forestalling has officially come to an end. The State recently enacted new physician standards for telemedicine practice, and the State legislature is presently considering further regulation. These new standards do not impinge upon the prior standards for telemedicine prescribing practice, but are issued in conjunction to it.
View original post 304 more words
Steps 1 and 2 (of 7) in Doing a Healthcare Deal (Correctly)
Step 1 – Describe and Understand the Deal
- Why?
- What is it that is hoped to be accomplished?
- Why is that a good outcome?
- Does it make sense? I.e., is it commercially reasonable?
- Is the deal more than just about referrals and money?
- What happens if a regulator “follows the money”?
- How will the deal affect others – patients, employees, physicians, competitors, the community, etc.?
- What are the tax effects?
- Engage legal, accounting, valuation, and other professional consultants early in the process to review the proposed deal.
Step 2 – Identify the Parties to the Deal
- Who is involved (medical professionals, background)?
- Why are they involved?
- What do they bring to the deal?
- When did they get involved?
- Who got them involved?
- What does each party hope to achieve?
- Are the goals reasonable?
- Are the goals legal and ethical?
Dos and Donts of Deal Making in Healthcare
Last week, I presented at a webinar sponsored by the American Association of Orthopaedic Executives. The topic dealt was “2014 Healthcare Compliance.” You can access the entire PowerPoint presentation at SlideShare.
I spoke about the dos and don’ts of healthcare deal making. The focus was on deals with physicians, but the concepts are applicable to deals involving all types of healthcare providers. Below I summarize my Rules of Thumb for healthcare deals:
Rules of Thumb for Healthcare Deals
- RULE #1: Just because a proposed deal makes sense and would be appropriate in a business other than healthcare, doesn’t mean it’s legal. (Corollary — Just because everyone is doing it, doesn’t mean it’s legal.)
- RULE #2: Determining the legality of a healthcare deal can be complicated, time consuming, expensive, and inconclusive.
- RULE #3: The risks of doing an illegal healthcare deal far outweigh the benefits.
- RULE #4: Get professional help early in the deal.
In subsequent posts, I will discuss steps in the deal and ways to screw up the deal.
The Need for Physician Leadership Development
It is critical now that medical practices take the steps needed “to retain, develop, and align [its] medical staff to meet the challenges of a fast-changing and highly competitive healthcare landscape.” Good physician leaders can help achieve those goals. This is the message in a recent post from Physicians Practice, “Medical Practices Must Focus on Physician Leadership Development.”
Equally important, however, is the need for physician leaders to see and develop opportunities as a result of forces in the very fast moving healthcare environment outside of their own medical practices.
Questions, like the following, are constantly swirling around medical practices, and I fear they are as often ignored as they are avoided:
- Should we align with the hospital?
- Should we join a large physician group?
- Should we develop our own super group?
- Should we join the hospital sponsored clinically integrated network?
- Should we start our own network?
Hospitals and venture capitalists have the money, the time, and the leadership to develop and pursue healthcare business opportunities, and they are doing so. They are taking the lead in presenting answers to these questions. Physicians are at a disadvantage, because they rarely have the money or the time or, unfortunately, the leadership to be proactive in evaluating and accepting or rejecting opportunities as they present themselves.
If survival as independent practices is the goal, then in this highly competitive business environment, physician leadership has never been more important. This has been the message of many physician practice commentators, including Kevin Pho, M.D. on his blog, as well as physician leadership training programs like the one done at the University of Cincinnati.
No one is waiting for physicians to step. When they do, they can control their professional destiny. When they don’t or can’t, others will be in control.